Gallbladder Problems with Gallstones: Understanding, Diagnosis, and Treatment
Gallbladder problems, particularly those caused by gallstones, are common yet often misunderstood. This article explores the nature of gallbladder issues, focusing on gallstones, their causes, symptoms, and the latest management techniques. If you or someone you know has been dealing with gallbladder discomfort, this comprehensive guide will be a valuable resource.
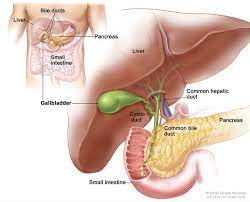
What Is the Gallbladder and What Are Gallstones?
The gallbladder is a small, pearshaped organ located under the liver. It stores bile, a digestive fluid produced by the liver. Gallstones, or cholelithiasis, are hardened deposits that can form in the gallbladder. They vary in size from as small as a grain of sand to as large as a golf ball.
A Historical Insight: Gallbladder Disease Over Time
Gallstones and gallbladder problems have been documented as far back as ancient Egypt, where gallstone findings were discovered in mummies. Over the centuries, advancements in medicine have allowed for a better understanding of these issues and more sophisticated treatment methods.
What Causes Gallstones to Form?
Gallstones develop when there is an imbalance in the substances that make up bile, leading to crystallization. Key factors include:
Excess Cholesterol: When bile contains too much cholesterol, it can crystallize and form stones.
Bile Concentration: When the gallbladder doesn’t empty completely, the bile can become concentrated and lead to stone formation.
Pigment Imbalance: High levels of bilirubin due to liver conditions can also contribute to stone development.
Recognizing the Symptoms of Gallbladder Problems
While some people experience silent gallstones without any symptoms, others may suffer from:
Severe Pain: Sudden and intense pain in the upper right abdomen or between the shoulder blades, known as biliary colic.
Nausea and Vomiting: Often accompanying episodes of pain.
Indigestion: Especially after fatty meals.
Jaundice: Yellowing of the skin and eyes if a stone obstructs the bile ducts.
How Is Gallbladder Disease Diagnosed?
Diagnosis begins with a physical examination and a detailed review of symptoms. The following tests are often recommended:
Ultrasound: The most common and noninvasive method to detect gallstones.
CT Scan: Useful for identifying complications or detecting stones in the bile ducts.
HIDA Scan: Assesses the function of the gallbladder.
Blood Tests: To check for infection or bile duct obstruction.
NonSurgical and Medical Management of Gallstones
In some cases, medical treatment may be an option:
Oral Medications: Certain drugs can dissolve small cholesterol stones over time.
Dietary Changes: Reducing fatty food intake to prevent triggering gallbladder pain.
Pain Management: Overthecounter or prescribed pain medications can help alleviate symptoms.
Home Remedies and Preventive Measures
While gallstones cannot always be prevented, there are lifestyle choices that can reduce risk:
Maintain a Healthy Weight: Obesity is a major risk factor for gallstones.
Eat a Balanced Diet: Highfiber foods and healthy fats help promote good digestion.
Stay Active: Regular exercise can aid in maintaining a healthy weight.
When Is Surgery Necessary?
Surgery is generally recommended if:
Gallstones are causing repeated or severe pain.
There is evidence of inflammation or infection in the gallbladder.
Stones are obstructing the bile ducts.
Surgical Options for Gallbladder Removal
- Laparoscopic Cholecystectomy: A minimally invasive surgery using small incisions to remove the gallbladder. This is the most common and preferred approach, resulting in a quicker recovery.
- Open Cholecystectomy: Sometimes necessary if complications are present, involving a larger incision to remove the gallbladder.
Preparing for Surgery: PreOperative Guidelines
Tests Required: Blood work, imaging scans, and cardiac assessments to ensure fitness for surgery.
Fasting Instructions: No food or drink for 6 to 8 hours before surgery to minimize anesthesia risks.
How Long Does Gallbladder Surgery Take?
Laparoscopic Surgery: Typically lasts between 30 to 45 minutes.
Open Surgery: May take up to 60 minutes, depending on the complexity.
PostOperative Recovery and Care
Hospital Stay: Laparoscopic patients often go home the same day, while open surgery patients may require a 1 to 2day hospital stay.
Diet PostSurgery: Start with liquids, gradually progressing to solid foods within 24 hours.
Activity Level: Gentle walking is encouraged soon after surgery, but avoid heavy lifting for at least 2 to 4 weeks.
Returning to Normal Life: When to Resume Activities
Most patients can return to work or daily activities within 1 to 2 weeks after laparoscopic surgery and 4 to 6 weeks after open surgery. Desk jobs may allow earlier resumption, but always consult your surgeon for personalized advice.
Complete Recovery Time
Laparoscopic Surgery: Complete recovery in about 2 to 3 weeks.
Open Surgery: Full recovery can take up to 6 weeks.
PostOperative FollowUp
At (https://www.surgeondrimtiazhussain.com), we offer comprehensive followup care. Local patients are advised to visit for checkups, while national and international patients can stay in touch through WhatsApp. Dr. Imtiaz Hussain personally monitors each patient’s recovery, reviewing wound progress and adjusting care plans when needed.
How to Contact Us for an Appointment
If you are experiencing symptoms of gallbladder disease or suspect you may have gallstones, don’t hesitate to contact us. For appointments, simply send your medical reports and any relevant details. Dr. Imtiaz Hussain will review your case and provide the necessary guidance for the best course of action.
Conclusion
Gallstones and gallbladder issues are manageable conditions with proper diagnosis and timely treatment. Whether it’s adopting preventive measures, seeking medical treatment, or opting for surgery, taking charge of your health is key. Don’t delay—contact an expert if you have concerns about your gallbladder.